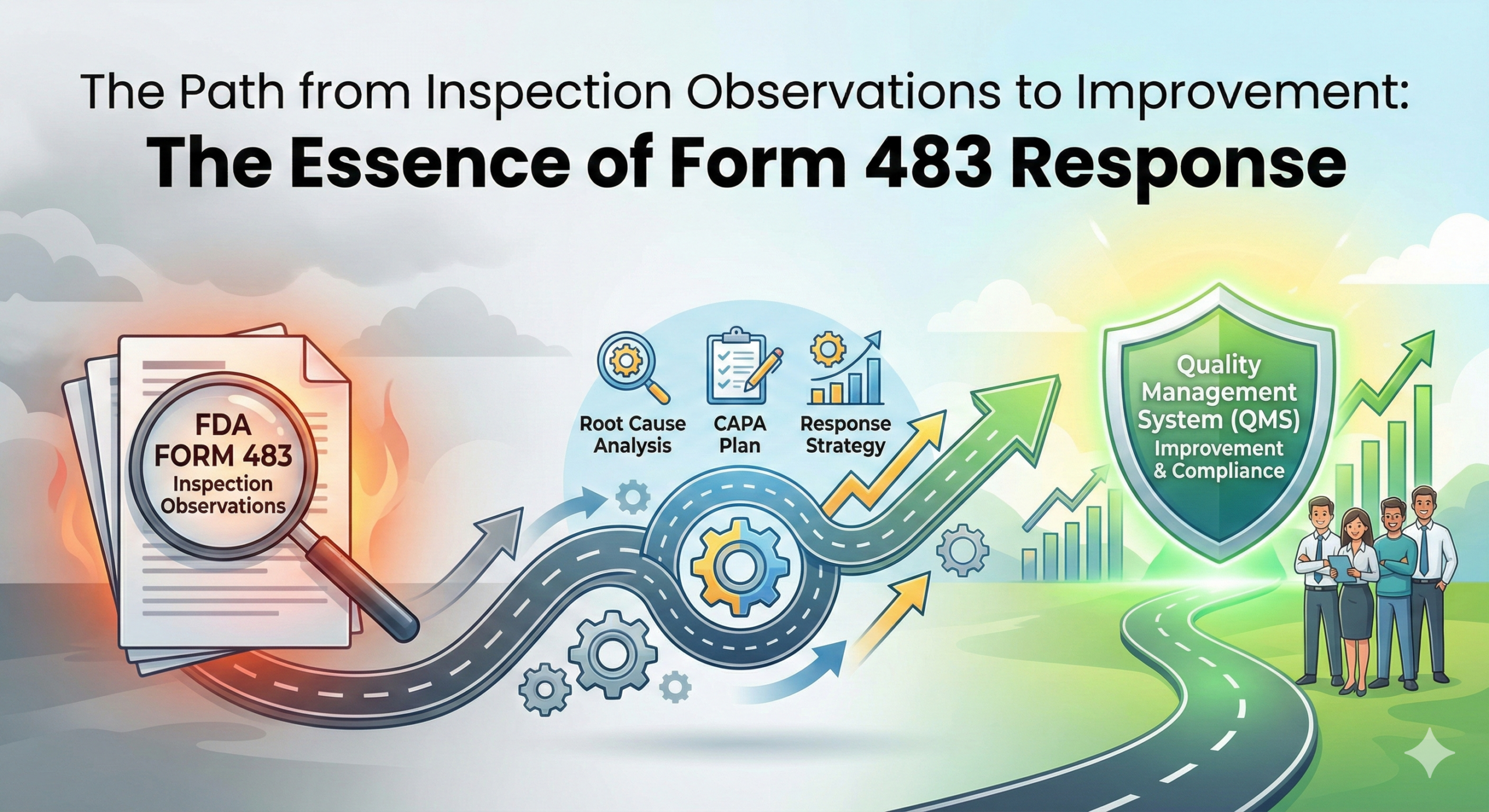
The Path from Inspection Observations to Improvement: The Essence of Form 483 Response
Introduction
In 2025, regulatory compliance in the pharmaceutical industry is at a critical turning point, transitioning from formal adherence to the cultivation of a genuine quality culture. Form 483, issued by the U.S. Food and Drug Administration (FDA), is no longer merely a document of observations but has evolved into a valuable diagnostic tool for fundamentally reviewing an organization’s quality management system.
Form 483 is an observation report that documents deviations from regulatory requirements discovered by FDA investigators during facility inspections. This document is presented on-site at the conclusion of an inspection, and companies are encouraged to respond within 15 business days. Critically, an appropriate response to Form 483 is key to avoiding the issuance of more serious Warning Letters.
The Essence of Form 483: Evolution Toward a Diagnostic Approach
Moving Beyond “Blind Compliance”
Until now, many companies have focused on formal compliance with regulatory requirements—what might be called “checkbox compliance.” However, regulatory authorities, including the FDA, are demanding not superficial responses but genuine improvements to quality systems. In 2025, true improvement means not merely treating symptoms but transforming the organization’s entire quality culture.
As outlined in ICH Q10 (International Conference on Harmonisation Quality Guidelines), an effective pharmaceutical quality system must ensure consistent quality throughout the product lifecycle and promote continuous improvement. This philosophy is reflected in PIC/S (Pharmaceutical Inspection Co-operation Scheme) GMP (Good Manufacturing Practice) guidelines and has become a global regulatory standard.
A New Perspective on Quality Management
Form 483 represents an important opportunity to reveal structural issues lurking within an organization’s quality control system. The observations are merely the tip of the iceberg, and thoroughly exploring the root causes behind them leads to genuine quality improvement.
Recent FDA trends show an increasing number of observations related to data integrity, computerized system validation, supply chain management, and quality risk management. These demonstrate the importance of practically applying the concepts of ICH Q9 (Quality Risk Management) and ICH Q8 (Pharmaceutical Development).
An Effective Improvement Plan: A Strategic Approach
Developing an effective improvement plan requires a systematic approach. The following six strategic steps outline how to achieve genuine quality improvement.
Step 1: Thorough Root Cause Analysis
From a CAPA (Corrective Action and Preventive Action) perspective, it is necessary to analyze the root causes of problems from multiple angles. ICH Q10 defines the CAPA system as a systematic approach for identifying, investigating, and taking appropriate action on product and process issues.
Root cause analysis employs methods such as the Five Whys, fishbone diagrams (Ishikawa diagrams), and FMEA (Failure Mode and Effects Analysis). During analysis, it is important to consider the following factors:
Human Factors: Insufficient training, skill gaps, lack of procedural understanding, inadequate awareness. It is essential not only to provide training but also to evaluate its effectiveness and confirm its application in practice.
Process Factors: Ambiguous procedures, inefficient workflows, process complexity, resource shortages. Through process mapping, workflows can be visualized to identify bottlenecks and improvement opportunities.
System Factors: Inadequate document management systems, structural problems in quality control systems, IT system constraints, organizational structure issues. Regarding data integrity in particular, system design must satisfy the ALCOA+ principles (Attributable, Legible, Contemporaneous, Original, Accurate, plus Complete, Consistent, Enduring, and Available).
Organizational Culture Factors: The degree of quality culture penetration, open communication, an environment that encourages reporting, management commitment. While these factors are difficult to quantify, they are indispensable for long-term quality improvement.
Step 2: Risk Assessment and Strategic Prioritization
Rather than treating all observations equally, priorities should be determined based on a risk-based approach. Following the risk management principles recommended by ICH Q9, evaluate from the following perspectives:
Impact on Patient Safety: This is the most important evaluation criterion. Problems that pose direct or potential health risks to patients must be addressed with the highest priority.
Potential Risk to Product Quality: Evaluate problems that may affect product efficacy, safety, or quality characteristics.
Regulatory Compliance Risk: Assess the severity of observations (Critical, Major, Minor) and consider the possibility of escalation to Warning Letters or Consent Decrees.
Resource Requirements and Effectiveness Evaluation: Estimate the time, personnel, financial resources, and technical resources needed for improvement and evaluate cost-effectiveness. However, for matters related to patient safety, cost should not take precedence.
Scope of Impact: Evaluate the possibility that the problem may spread to other product lines, facilities, or processes.
Risk assessment commonly uses a risk matrix (two-dimensional evaluation of probability and impact). This allows risk levels to be visualized and creates shared understanding among stakeholders.
Step 3: Developing a Strategic and Specific Improvement Plan
Rather than a formal response plan, create a concrete roadmap that transforms the organization’s quality culture. An effective improvement plan includes the following elements:
Defining Clear and Measurable Improvement Actions: Rather than vague expressions (“improve,” “strengthen”), describe specific, observable actions. For example, “Conduct four hours of hands-on data integrity training for all manufacturing operators and confirm understanding with test scores of 80% or higher.”
Clarifying Specific Roles and Authority of Responsible Parties: Use a RACI matrix (Responsible, Accountable, Consulted, Informed) to clearly define responsibility for each action.
Setting Achievable and Realistic Deadlines: Categorize into immediate response, short-term (30-60 days), medium-term (3-6 months), and long-term (6+ months), and establish a phased implementation plan. FDA responses require specific completion dates.
Establishing Quantitative Improvement Indicators: Set Key Performance Indicators (KPIs) or Key Quality Indicators (KQIs) to measure improvement progress and effectiveness. Examples include deviation occurrence rates, CAPA completion rates, training implementation rates, and quality review implementation rates.
Building Progress Tracking Systems: Establish a management framework to ensure the improvement plan is executed, including regular review meetings, progress report formats, and escalation processes.
Verification of Corrective Action Effectiveness: Include a process to verify that improvement measures actually solved the problem. This includes setting post-implementation monitoring periods, methods for measuring effectiveness, and criteria for determining when additional measures are needed.
Step 4: Cultivating a Comprehensive Quality Culture Throughout the Organization
Quality improvement is not the responsibility of a specific department but the mission of the entire organization. To cultivate a genuine quality culture, the following initiatives are necessary:
Clear and Strong Commitment from Senior Management: Quality culture cannot be realized without commitment from top management. Senior leadership must demonstrate dedication to quality not just through words but through resource allocation, decision-making, and daily actions. ICH Q10 explicitly states management responsibilities including establishing quality policy, setting quality objectives, and conducting management reviews.
Establishing Cross-Functional Quality Improvement Working Groups: Assemble cross-functional teams with members from all relevant departments including manufacturing, quality control, quality assurance, R&D, supply chain, IT, and regulatory affairs. This prevents siloing and drives consistent improvement across the organization.
Implementing Continuous Education Programs: Conduct regular training on GMP, data integrity, quality risk management, root cause analysis methods, etc. Training should not be one-time but should provide ongoing learning and skill development opportunities. Follow-up to evaluate training effectiveness and confirm practical application is also necessary.
Building an Open and Transparent Communication Culture: Cultivate a culture that encourages early reporting and sharing of problems rather than hiding them. This includes implementing non-punitive reporting systems (Just Culture), regular quality meetings, and platforms for sharing quality information.
Visualizing and Sharing Quality Metrics: Visualize quality indicators on dashboards and share them across the organization. This allows everyone to understand the current situation and feel the progress of improvements.
Step 5: Continuous Monitoring and Dynamic Improvement
Improvement is not a one-time event but a process of sustained evolution. As emphasized by ISO 9001 (Quality Management Systems) and ICH Q10, it is important to continuously cycle through Plan-Do-Check-Act (PDCA).
Implementing Real-Time Quality Monitoring Systems: Utilize Manufacturing Execution Systems (MES) and electronic batch record systems to monitor manufacturing processes in real-time. When abnormalities are detected, immediately issue alerts to enable rapid response.
Conducting Regular and Thorough Internal Audits: Plan internal audits based on a risk-based approach, conducting audits more frequently in high-risk areas. Internal audits are an important tool not only for preparing for external inspections but also for identifying continuous improvement opportunities. PIC/S GMP guidelines require the establishment of quality audit programs.
Ensuring Transparency of Improvement Progress: Maintain transparency of improvement activities through regular status reports, management reviews, and progress sharing with relevant departments.
Data-Driven Continuous Improvement Approach: Analyze quality data, understand trends, and conduct proactive management. Advanced companies are also adopting Statistical Process Control (SPC), big data analysis, and predictive analytics using artificial intelligence.
Utilizing Annual Product Review/Product Quality Review: Aggregate data annually for each product to evaluate overall quality status. This allows understanding of long-term trends and identification of systematic problems.
Step 6: Preventive Approach and Organizational Learning
Rather than ending with one-off responses, institutionalize organizational learning and preventive management. This is based on the concepts of “continuous improvement” and “knowledge management” advocated by ICH Q10.
Systematic Documentation of Lessons Learned: Systematically document Form 483 observations, root cause analysis results, improvement measures implemented, and their effectiveness, accumulating them as the organization’s knowledge base. Horizontally deploy lessons to prevent recurrence of similar problems.
Continuous Self-Improvement Mechanisms for Quality Management Systems: Build mechanisms to continuously evolve the quality system itself, including regular system reviews, process improvement proposal systems, benchmarking, and incorporation of industry best practices.
Institutionalizing and Deploying Preventive Measures: Learn from problems discovered in one product line or facility and deploy preventive measures to other areas. This allows addressing issues before they manifest.
Building Knowledge Management Systems: Build systems to systematically manage and share organizational knowledge and experience. This includes continuous improvement of Standard Operating Procedures (SOPs), platforms for sharing technical information, and building expert networks. ICH Q10 positions knowledge management as an important element of quality systems.
Continuous Monitoring of Industry Trends and Regulatory Information: Understand the latest regulatory trends and industry best practices through FDA guidance documents, industry white papers, professional journals, and conferences, and take proactive action.
The Essential Approach to Avoiding Warning Letters
An appropriate response to Form 483 is extremely important for avoiding the issuance of more serious Warning Letters. A Warning Letter is an official notification document that the FDA issues when significant regulatory violations are discovered and not corrected. This not only severely impacts a company’s reputation but can also lead to enforcement actions such as import bans, manufacturing halt orders, and civil or criminal litigation.
Formal responses are insufficient. The true solution to avoiding Warning Letters is the transformation of the organization’s fundamental quality culture. According to FDA statistics, many companies that receive Warning Letters had insufficient responses to Form 483 or failed to implement promised improvement measures.
Regulatory authorities seek not superficial corrections but sincere commitment to quality from the entire organization. This includes the following elements:
Timely and Sincere Response: It is recommended to submit a detailed and specific response within 15 business days of receiving Form 483. The response should clearly state acknowledgment of observations, root cause analysis results, specific corrective actions, preventive actions, completion dates, and responsible parties.
Fulfilling Commitments: Reliably implement improvement measures promised in the response according to schedule. If progress is delayed, explain the reasons and submit a revised plan. The FDA carefully monitors whether commitments are kept.
Continuous Communication: Continue dialogue with the FDA as needed. For complex improvement measures, pre-operational visits or requests for guidance can also be considered.
Voluntary Improvements: Voluntarily extend improvements not only to pointed-out matters but also to related areas. This serves as evidence that the company is seriously committed to quality improvement.
Global Perspective: Harmonization with International Regulations
The pharmaceutical industry is increasingly globalized, requiring compliance with regulations from multiple countries and regions. Mechanisms similar to FDA Form 483 are adopted by other regulatory authorities.
EMA (European Medicines Agency) and PIC/S: In inspections by PIC/S member states, a Statement of Non-Compliance may be issued. PIC/S GMP guidelines are fundamentally harmonized with EU GMP, WHO GMP, and FDA GMP, making it possible to build internationally applicable quality systems.
PMDA (Pharmaceuticals and Medical Devices Agency): In Japan, when GMP non-compliance is discovered in conformity assessments conducted by PMDA, it is notified as an observation. Japan’s GMP ministerial ordinance has been revised based on international standards such as ICH Q7 (API GMP Guidelines), ensuring consistency with global standards.
Other Regulatory Authorities: Health Canada, Australia’s TGA (Therapeutic Goods Administration), and China’s NMPA (National Medical Products Administration) also have their respective inspection systems.
By building a global quality system, companies can efficiently respond to the requirements of multiple regulatory authorities. Quality systems based on ICH guidelines serve as a foundation accepted worldwide.
Utilizing Digital Technology: Evolution Toward Quality 4.0
As of 2025, digitalization in pharmaceutical manufacturing is rapidly progressing. The concepts known as “Pharma 4.0” and “Quality 4.0” are attracting attention, and innovation in quality management utilizing digital technology is advancing.
Electronic Quality Management Systems (eQMS): Implementation of electronic systems integrating document management, change management, deviation management, and CAPA management realizes improved operational efficiency and transparency.
Ensuring Data Integrity: System design compliant with 21 CFR Part 11 (Electronic Records and Electronic Signatures) and Annex 11 (EU GMP Computerized Systems) ensures data integrity. Audit trails, access control, backup, and disaster recovery are important.
Artificial Intelligence and Machine Learning: Attempts to utilize AI and machine learning for manufacturing data analysis, quality prediction, and anomaly detection are increasing. This enables preventive quality control.
Digital Twins: Technology for building digital twins of manufacturing processes and conducting simulations and optimization is also being researched.
Blockchain: Blockchain technology is being considered for ensuring supply chain transparency and traceability.
These digital technologies have the potential to dramatically improve the efficiency and effectiveness of quality control, but they also create new regulatory challenges. Appropriate management of computerized system validation (CSV), data integrity, and cybersecurity is essential.
Conclusion: The Path to Quality Excellence
Form 483 is not a document to be feared but a valuable opportunity to fundamentally strengthen organizational quality. In the pharmaceutical industry of 2025, the essence of regulatory compliance lies in the evolution from “compliance” to “quality excellence.”
Rather than formally processing observations, it is important to evolve the organization’s quality culture itself. Through this transformation process, companies can achieve true quality management beyond mere regulatory compliance.
Effective quality management protects patient safety, ensures product quality, and supports sustainable corporate growth. As ICH Q10 indicates, pharmaceutical quality systems must be based on science and risk-based approaches, ensuring product quality throughout the product lifecycle and promoting continuous improvement.
Taking regulatory compliance as an opportunity for growth and learning with a forward-looking attitude and maintaining an attitude of continuous evolution will be the key to pharmaceutical quality management going forward. When the entire organization takes responsibility for quality, makes data-driven decisions, and takes a preventive approach, a genuine quality culture is cultivated.
Finally, it must not be forgotten that quality is not a destination but a journey. There is no perfect quality system, and there is always room for improvement. The attitude of learning humbly, working sincerely, and doing one’s best for patients is the fundamental value required of all those engaged in the pharmaceutical industry.

Comment