The Fundamental Structure of FDA Inspections: Safeguarding Quality and Safety in Healthcare and Pharmaceutical Industries
In the world of healthcare and pharmaceuticals, inspections conducted by the FDA (Food and Drug Administration) represent an extremely important process for ensuring product safety and quality. This article will explain the overall picture of FDA inspections and their important mechanisms in a way that is easy to understand, even for beginners.
What Are FDA Inspections?
FDA inspections are comprehensive audit processes to verify that companies involved in the manufacturing and distribution of pharmaceuticals, medical devices, food, cosmetics, and other products comply with legal regulations and safety standards. They are not mere checklist confirmations but crucial initiatives that evaluate product safety and quality from multiple perspectives.
Types of Inspections
FDA inspections primarily consist of the following four types:
1. Pre-Approval Inspection (PAI)
Pre-Approval Inspections are critical evaluations conducted before new drug approval to confirm the suitability of manufacturing facilities. According to the latest FDA guidance (Compliance Program 7346.832, updated to reflect ICH Q9, Q10, and Q12 guidelines), PAIs now focus on four main objectives:
- Objective 1: Readiness for Commercial Manufacturing – Determine whether the establishment has a quality system designed to achieve sufficient control over the facility and commercial manufacturing operations
- Objective 2: Conformance to Application – Verify that formulation, manufacturing or processing methods, and analytical methods are consistent with descriptions in the Chemistry, Manufacturing, and Controls (CMC) section of the application
- Objective 3: Data Integrity Audit – Audit raw data (hardcopy or electronic) to authenticate the data submitted in the CMC section of the application
- Objective 4: Commitment to Quality in Pharmaceutical Development – Assess the applicant’s commitment to quality throughout the pharmaceutical development process
These inspections are essential processes conducted before commercial production of new drugs and increasingly emphasize data integrity and the relationship between submitted data and operational reality.
2. Routine Surveillance Inspection
Since the Food and Drug Administration Safety and Innovation Act (FDASIA) of 2012, FDA has implemented a risk-based approach to determine inspection frequency, replacing the previous statutory biennial (two-year) inspection cycle. While many establishments are still inspected approximately every two to three years based on risk assessment, the frequency now depends on various risk factors including:
- Facility type (manufacturer, control laboratory, etc.)
- Compliance history and whether inspected within the last four years
- Hazard signals and recall history
- Inherent product risks (dosage form, route of administration, sterility requirements, etc.)
- Recognition of inspections by foreign regulatory partners through Mutual Recognition Agreements (MRAs)
These inspections comprehensively evaluate a company’s ongoing quality management system and may be conducted with or without advance notice. The purpose is to verify continuous compliance with current Good Manufacturing Practice (cGMP) requirements.
3. Good Clinical Practice (GCP) Inspection (Clinical Trial Inspection)
GCP inspections evaluate the ethical conduct and scientific validity of clinical trials. According to recent data (2017-2023), FDA completed approximately 2,836 review-based routine GCP inspections in support of marketing applications, with final classification outcomes of:
- No Action Indicated (NAI): 81.2%
- Voluntary Action Indicated (VAI): 18.5%
- Official Action Indicated (OAI): 0.3%
These inspections are typically conducted within six months after New Drug Application (NDA) submission, with three to four Phase III trial sites commonly selected. They confirm the protection of subjects’ safety and rights and are classified into:
- Routine Inspection: Regularly scheduled inspections for marketing applications
- Directed Inspection: Targeted inspections based on specific concerns
4. For-Cause Inspection
For-cause inspections are emergency inspections conducted in response to specific problems, complaints, accidents, or other triggers. They differ significantly from routine surveillance in both scope and intensity, requiring immediate response and detailed investigation. These are highly flexible inspections implemented for cases with high urgency, where investigators arrive with specific concerns to address and conduct deep investigations into related systems and processes.
Classification of Inspection Results
FDA inspection results are classified into the following three categories:
- NAI (No Action Indicated): No regulatory action required; the facility demonstrates satisfactory compliance
- VAI (Voluntary Action Indicated): Voluntary improvement needed; objectionable conditions observed but do not meet the threshold for regulatory action
- OAI (Official Action Indicated): Official regulatory action required; significant violations that may lead to enforcement action
Focus Points of FDA Investigators
FDA investigators focus on the following important points during their investigations:
- Accuracy and transparency of document management
- Consistency of quality management systems
- Standardization of manufacturing processes
- Data integrity (completeness and reliability of data)
- Risk management processes
- Ensuring traceability
- Compliance with ICH guidelines (Q9 Quality Risk Management, Q10 Pharmaceutical Quality System, Q12 Lifecycle Management)
- Knowledge management practices
- Supply chain control and oversight of outsourced activities
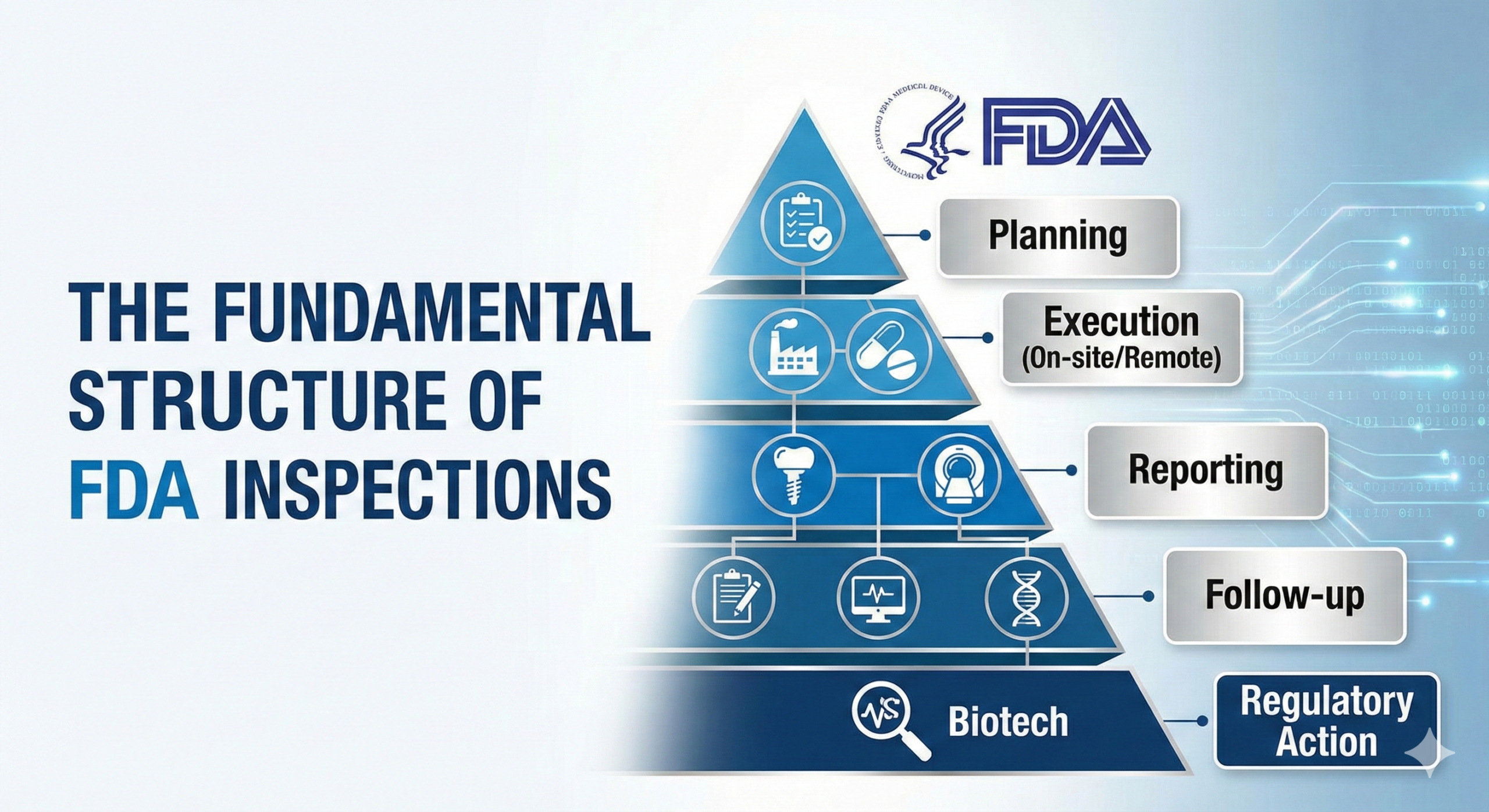
Overall Picture of the Inspection Process
Pre-Inspection Preparation Stage
- Receipt of inspection notice (with advance notice or unannounced)
- Organization of relevant documents
- Explanation to internal teams and role assignment
- Review of applicable ICH guidelines and current regulations
- Preparation of key personnel for interviews
Inspection Implementation Stage
- Opening meeting
- Document review
- On-site inspection
- Interviews and detailed confirmation
- Sharing of preliminary findings
- Closeout meeting with presentation of observations
Post-Inspection Response Stage
- Receipt of Form 483 listing inspectional observations
- Preparation of corrective action plan (Response Letter)
- Submission of response to FDA District Office within 15 business days from the date Form 483 was issued
- Implementation of corrective and preventive actions (CAPA)
- Follow-up reporting and potential re-inspection to verify corrective actions
Important Note on Response Timeline: According to FDA policy established in 2009 and reinforced through subsequent guidance, firms are strongly encouraged to provide a written response to Form 483 observations within 15 business days. The timeline begins the day after Form 483 is issued. Business days exclude Saturdays, Sundays, and federal holidays. Failure to respond within this timeframe may result in FDA moving toward more serious enforcement action, such as issuing a Warning Letter. The response must include root cause analysis, immediate corrections, preventive actions, and realistic timelines for completion.
Latest Inspection Trends
The FDA has modernized its inspection approach to reflect current regulatory science and global manufacturing realities:
- Risk-Based Inspection Approach: Implementation of the Site Selection Model (SSM) prioritizing high-risk facilities
- Formal Introduction of Systems-Based Inspection: Since 2002, FDA has formally adopted systems-based inspection approaches that evaluate entire quality systems rather than isolated components
- Intensive Focus on Data Integrity: Enhanced scrutiny of data lifecycle management, from raw data generation through final reporting
- Integration of ICH Guidelines:
- ICH Q9(R1) (2023): Revised Quality Risk Management guideline emphasizing hazard identification, risk review, and formality in QRM
- ICH Q10 (2008): Pharmaceutical Quality System guideline promoting lifecycle approach
- ICH Q12 (2021): Technical and Regulatory Considerations for Pharmaceutical Product Lifecycle Management
- Alternative Assessment Tools: Introduction of Remote Regulatory Assessments (RRAs) and Remote Interactive Evaluations (RIEs) as supplements to traditional on-site inspections
- Mutual Recognition Agreements (MRAs): FDA increasingly recognizes inspections conducted by foreign regulatory partners, though to date, PAIs/PLIs conducted by foreign authorities have not been recognized
- Quality Management Maturity (QMM) Program: FDA’s initiative (launched 2022) to assess pharmaceutical quality systems based on attributes aligned with ICH Q10
Practical Advice for Inspection Preparation
To successfully navigate FDA inspections, organizations should:
- Maintain Current Regulatory Awareness: Stay updated on the latest regulatory requirements, including FDA guidance documents, ICH guidelines, and industry best practices
- Establish Robust Document Management Systems: Implement comprehensive documentation practices that ensure data integrity, traceability, and regulatory compliance
- Conduct Regular Internal Training: Provide ongoing training to all staff on cGMP requirements, company SOPs, and inspection preparedness
- Share Risk Management Awareness Organization-Wide: Foster a culture of quality where risk management principles (ICH Q9) are embedded in daily operations
- Implement Strong Quality Systems: Develop and maintain a Pharmaceutical Quality System aligned with ICH Q10 principles
- Establish Knowledge Management Practices: Create systems to capture, share, and apply knowledge throughout the product lifecycle
- Conduct Mock Inspections: Regular simulation exercises conducted by experienced professionals to identify gaps and improve readiness
- Maintain Inspection Readiness Continuously: Operate as if an inspection could occur at any time, particularly for facilities subject to unannounced inspections
- Develop Clear Communication Protocols: Establish roles, responsibilities, and communication chains for when inspectors arrive
- Ensure Senior Management Engagement: Quality oversight and inspection preparedness should be priorities at the executive level
Conclusion
FDA inspections are not threats to companies but valuable opportunities to continuously improve product quality and safety. Appropriate preparation and a positive attitude are the keys to successful inspections.
The insights gained through inspections contribute not only to regulatory compliance but also significantly to the organization’s sustainable growth and enhancement of credibility. By embracing a proactive approach to quality and viewing inspections as catalysts for improvement, pharmaceutical and medical device manufacturers can strengthen their operations, protect public health, and maintain competitive advantages in the global marketplace.
As the regulatory landscape continues to evolve with new guidelines, technologies, and global harmonization efforts, organizations that invest in robust quality systems aligned with ICH principles and FDA expectations will be best positioned for long-term success. The integration of quality risk management, knowledge management, and lifecycle approaches represents the future of pharmaceutical quality assurance—one where inspection readiness is not a periodic activity but a continuous state of operational excellence.
Note: This article reflects regulatory requirements and guidance as of January 2026. Regulations and guidance documents are subject to change. Organizations should always consult the most current FDA guidance documents, Federal Register notices, and ICH guidelines for the latest requirements.

Comment