Reflections on the Revised GMP Ministerial Ordinance: From Standards to Professional Practice
Understanding GMP: More Than Just an Acronym
As is well known, GMP stands for “Good Manufacturing Practice.” A literal translation would be “Good Manufacturing Practice” or “Practical Manufacturing Standards.” However, in Japan, the Ministry of Health, Labour and Welfare (MHLW) ordinance is officially titled “Ministerial Ordinance on Standards for Manufacturing Control and Quality Control of Drugs and Quasi-Drugs” (医薬品及び医薬部外品の製造管理及び品質管理の基準に関する省令).
I believe this title should be reconsidered in the context of the revised GMP ministerial ordinance. Why? Because even within the category of pharmaceuticals, the “standards” should differ between products such as vitamin supplements and nutritional drugs versus anticancer agents, psychotropic drugs, and antiviral medications.
The Evolution of GMP: From Prescriptive Standards to Risk-Based Approaches
Historical Context: The Birth of Regulatory Standards
GMP was first introduced by the U.S. Food and Drug Administration (FDA) in 1963 as a formal regulation. At that time, it truly provided specific “standards” – prescriptive requirements that manufacturers were expected to follow uniformly. This approach made sense in an era when the pharmaceutical industry was less complex and regulatory science was still developing.
The 1963 regulations represented a watershed moment in pharmaceutical quality assurance, establishing baseline expectations for facilities, equipment, records, and quality control. These rules were born from tragic incidents, including the 1937 sulfanilamide disaster that claimed over 100 lives and the 1941 sulfathiazole contamination incident. Such tragedies underscored the critical need for systematic manufacturing controls.
The Paradigm Shift: Risk-Based Regulation in the 21st Century
However, a fundamental transformation occurred when the FDA announced its “Pharmaceutical CGMPs for the 21st Century: A Risk-Based Approach” initiative in August 2002. This initiative marked a decisive shift in regulatory philosophy. Under this new paradigm, regulatory authorities no longer prescribe uniform “standards” for all products and processes. Instead, pharmaceutical companies must establish their own appropriate controls based on the specific risks associated with their products and manufacturing processes.
To implement this risk-based approach effectively, companies must conduct comprehensive risk assessments in accordance with ICH Q9 “Quality Risk Management” (first published in November 2005, revised as ICH Q9(R1) effective July 26, 2023) and document their findings thoroughly. Furthermore, companies must be prepared to justify to regulatory authorities that their established controls are appropriate and adequate for ensuring product quality and patient safety.
This represents a profound shift in responsibility – from following prescriptive regulations to developing science-based, risk-proportionate control strategies that may vary significantly depending on the product’s therapeutic category, formulation complexity, patient population, and manufacturing technology employed.
The Rationale: Patient-Centric Economics and Scientific Progress
The primary driver for transitioning to a risk-based approach is the reduction of patient burden through more efficient resource allocation. Imposing identical “standards” on all pharmaceuticals and manufacturing processes is not only scientifically unjustifiable but also unnecessarily inflates compliance costs. These increased costs ultimately translate to higher drug prices, reduced access to medicines, and potential barriers to innovation.
Consider the stark differences in risk profiles: A vitamin supplement manufactured through straightforward compression presents fundamentally different quality risks than a complex biologic anticancer agent requiring aseptic processing, cold chain management, and specialized handling. Applying identical control measures to both scenarios wastes resources that could be better deployed to address genuine risks.
The risk-based approach enables:
Proportionate Resource Allocation: Companies can focus intensive controls and monitoring on high-risk processes (such as sterile manufacturing of injectable oncology products) while applying streamlined, science-based controls to lower-risk operations (such as solid oral dosage forms of stable compounds). This optimization reduces unnecessary compliance costs without compromising patient safety.
Enhanced Innovation: By eliminating prescriptive barriers, the risk-based framework encourages adoption of advanced manufacturing technologies, continuous improvement initiatives, and process analytical technologies (PAT). Companies can justify changes and improvements based on scientific understanding rather than rigid regulatory prescriptions.
Global Harmonization: The risk-based approach, championed through ICH guidelines and adopted by major regulatory authorities worldwide including the FDA, European Medicines Agency (EMA), and Japan’s Pharmaceuticals and Medical Devices Agency (PMDA), facilitates international trade and reduces duplicative requirements across markets.
Professional Accountability in Modern GMP
Beyond Convenience: The Professional Imperative
From the perspective of pharmaceutical companies, having regulatory authorities prescribe specific “standards” may seem more convenient for daily operations. It provides clear boundaries and reduces decision-making uncertainty. However, this convenience-oriented mindset fundamentally misunderstands the nature of GMP as “Good Manufacturing Practice” – a professional practice framework rather than a prescriptive checklist.
Professional pharmaceutical manufacturing demands that companies and their personnel possess deep scientific knowledge, exercise sound judgment, and take ownership of quality decisions. This professional approach cannot be achieved by simply following prescribed standards without understanding the underlying scientific rationale. Such a superficial, amateur approach to compliance cannot adequately protect patient safety or ensure product quality.
Key Elements of Professional GMP Practice
Science-Based Decision Making: Modern GMP requires pharmaceutical professionals to understand the science underlying their processes, conduct meaningful risk assessments, and establish controls based on product and process knowledge rather than blind adherence to prescriptive standards. This demands continuous learning, critical thinking, and application of pharmaceutical science principles.
Quality Risk Management (QRM): As outlined in ICH Q9(R1), effective QRM requires systematic identification of hazards, analysis of risks, evaluation against acceptance criteria, implementation of proportionate controls, and ongoing review. This is not a one-time exercise but an integrated component of the pharmaceutical quality system throughout the product lifecycle. The 2023 revision of ICH Q9 particularly emphasizes managing subjectivity in risk assessments, addressing supply chain risks, and ensuring risk-based decision-making is properly implemented.
Pharmaceutical Quality System (PQS): ICH Q10 “Pharmaceutical Quality System” provides a comprehensive model that integrates GMP requirements with quality management principles and emphasizes knowledge management throughout the product lifecycle – from pharmaceutical development through commercial manufacturing and product discontinuation. A robust PQS enables companies to consistently deliver products of intended quality while facilitating continual improvement.
Documentation and Justification: Companies must thoroughly document their risk assessments, control strategies, and the scientific rationale supporting their approaches. This documentation serves not only for internal knowledge management but also to demonstrate to regulatory authorities during inspections that the company’s quality system is effective, science-based, and continuously improving.
The Japanese Context: Recent GMP Revision and International Harmonization
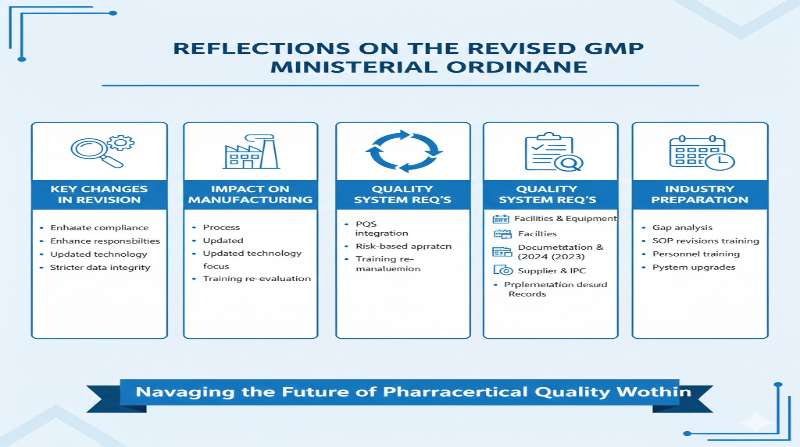
The 2021 Revision
Japan’s GMP ministerial ordinance underwent significant revision in April 2021 (effective August 1, 2021), representing the most substantial update in 16 years. This revision was undertaken to achieve greater international harmonization, particularly with PIC/S (Pharmaceutical Inspection Co-operation Scheme) GMP guidelines, which have become the de facto international standard. Japan officially joined PIC/S in July 2015, alongside the MHLW, Pharmaceuticals and Medical Devices Agency (PMDA), and prefectural authorities.
The revision incorporated several critical enhancements aligned with international best practices:
Pharmaceutical Quality System (PQS): Formalized requirements for comprehensive quality systems that integrate quality planning, knowledge management, and continual improvement throughout the product lifecycle, consistent with ICH Q10.
Quality Risk Management: Explicit requirements for systematic application of risk management principles, aligning with ICH Q9, to support science-based decision-making across all GMP activities.
Product Quality Review: Enhanced requirements for periodic comprehensive reviews of manufactured products to verify process consistency, identify trends, and drive continuous improvement.
Change Control and Deviation Management: Strengthened requirements for evaluating and managing changes and deviations, ensuring that quality impact is thoroughly assessed.
Knowledge Management: Formal recognition of the importance of capturing, maintaining, and utilizing knowledge gained throughout the product lifecycle to improve manufacturing and control strategies.
These enhancements represent Japan’s commitment to aligning with international GMP standards while maintaining rigorous oversight appropriate for protecting public health.
Balancing International Standards with Domestic Requirements
While pursuing international harmonization, Japanese regulations must continue to fulfill their domestic mandate of ensuring drug quality, efficacy, and safety for Japanese patients. The challenge lies in achieving harmonization without compromising the rigor necessary for public health protection. The revised GMP ordinance attempts this balance by adopting international frameworks (such as ICH Q9 and Q10) while retaining Japanese-specific requirements where scientifically justified.
Japanese pharmaceutical manufacturers now operate in a truly global regulatory environment, where compliance with domestic GMP requirements must harmonize with international expectations from PIC/S, FDA, EMA, and other authorities. This necessitates sophisticated quality systems capable of meeting multiple regulatory frameworks simultaneously.
The Path Forward: Embracing Professional Practice
Reconsidering Regulatory Terminology
Returning to my initial point, the current title of Japan’s GMP ordinance – “Ministerial Ordinance on Standards for Manufacturing Control and Quality Control” – may no longer accurately reflect the modern risk-based regulatory philosophy. The term “standards” (基準) implies uniformity and prescription, whereas contemporary GMP emphasizes customized, risk-based approaches tailored to specific products and processes.
A title emphasizing “practice” (実践) rather than merely “standards” would better capture the professional, judgment-based nature of modern pharmaceutical quality assurance. This is not mere semantics – language shapes understanding and mindset. If regulations are framed as prescriptive “standards,” companies may approach compliance mechanically rather than thoughtfully.
Building Professional Capability
The transition to risk-based GMP requires significant investment in professional development:
Education and Training: Personnel at all levels must understand not just what procedures to follow, but why those procedures matter, how to assess risks, and when adjustments may be warranted. This requires ongoing training in pharmaceutical science, quality risk management, and regulatory expectations.
Cross-Functional Collaboration: Effective risk assessment requires input from multiple disciplines – formulation scientists, process engineers, quality assurance professionals, regulatory experts, and manufacturing operators. Breaking down organizational silos enables more comprehensive risk identification and more robust control strategies.
Continuous Improvement Culture: Professional GMP practice embraces continual improvement through knowledge management, post-market surveillance, periodic review of manufacturing experience, and proactive identification of enhancement opportunities. This goes beyond mere compliance to pursue excellence in pharmaceutical quality.
Regulatory Intelligence: Companies must maintain awareness of evolving international standards, emerging technologies, scientific advances, and regulatory expectations across multiple jurisdictions. This requires dedicated resources for monitoring, interpretation, and implementation of relevant guidance.
The Role of Regulatory Authorities
Regulatory authorities also face challenges in the risk-based paradigm. Rather than simply verifying compliance with prescriptive standards, inspectors must assess whether companies have conducted meaningful risk assessments, established appropriate controls, and built effective quality systems. This requires:
Enhanced Inspector Training: Regulators need sophisticated training in quality risk management, pharmaceutical technology, and critical evaluation of company risk assessments and control strategies.
Flexible Inspection Approaches: Rather than checklist-based inspections, modern GMP oversight employs systems-based approaches that evaluate the effectiveness of the overall quality system in ensuring consistent product quality.
Dialogue and Guidance: As standards become less prescriptive, dialogue between industry and regulators becomes more important. Guidance documents, Q&A compendia, and consultation mechanisms help ensure shared understanding of expectations.
International Collaboration: Through mechanisms like PIC/S, regulatory authorities share inspection findings, harmonize expectations, and build mutual recognition of inspection outcomes, reducing duplicative oversight while maintaining high standards.
Conclusion: Professional Practice in the Service of Patient Safety
The evolution of GMP from prescriptive standards to risk-based professional practice represents maturation of pharmaceutical regulation. This approach recognizes that meaningful quality assurance cannot be achieved through rigid adherence to uniform standards but requires scientific understanding, professional judgment, and ongoing commitment to improvement.
For pharmaceutical companies, this transition demands elevation from following instructions to exercising professional expertise. It requires investment in knowledge, systems, and culture that may not always be convenient but is essential for fulfilling the fundamental obligation to patients: ensuring that medicines are consistently safe, effective, and of high quality.
The reduction of patient burden – through more affordable medicines enabled by efficient resource allocation and through enhanced availability enabled by reduced barriers to innovation – makes this professional approach not merely desirable but ethically imperative.
As the industry continues to evolve with advancing technology, increasing global complexity, and emerging therapeutic modalities, the risk-based professional practice paradigm provides the flexibility and rigor necessary to meet future challenges while maintaining unwavering focus on patient safety and product quality.
This is the essence of Good Manufacturing Practice in the 21st century – not amateur reliance on prescribed standards, but professional mastery in service of public health.
Author’s Note: The perspectives expressed in this column represent the author’s professional views on GMP regulatory philosophy and should not be construed as official guidance or legal advice. Companies should consult current regulations and seek appropriate professional advice for specific compliance matters.
References:
- FDA (2004). Pharmaceutical CGMPs for the 21st Century – A Risk-Based Approach
- ICH Q9 Quality Risk Management (November 2005)
- ICH Q9(R1) Quality Risk Management (January 2023, effective July 2023)
- ICH Q10 Pharmaceutical Quality System
- MHLW (2021). Ministerial Ordinance on Standards for Manufacturing Control and Quality Control of Drugs and Quasi-Drugs (Revised April 28, 2021, effective August 1, 2021)
- PIC/S GMP Guide for Medicinal Products
Related Articles
- Is Senior Management Responsible for GMP Compliance?
- The Importance of Supplier Management (Revised Edition)
- The Future of Japan’s GDP (Good Distribution Practice)
- Revision of Japan’s GMP Ministerial Ordinance
- Quality Manuals in Pharmaceutical Manufacturing: A Comprehensive Guide
Related FDA QMSR Templates
Streamline your FDA QMSR compliance with our professionally crafted templates:

Comment