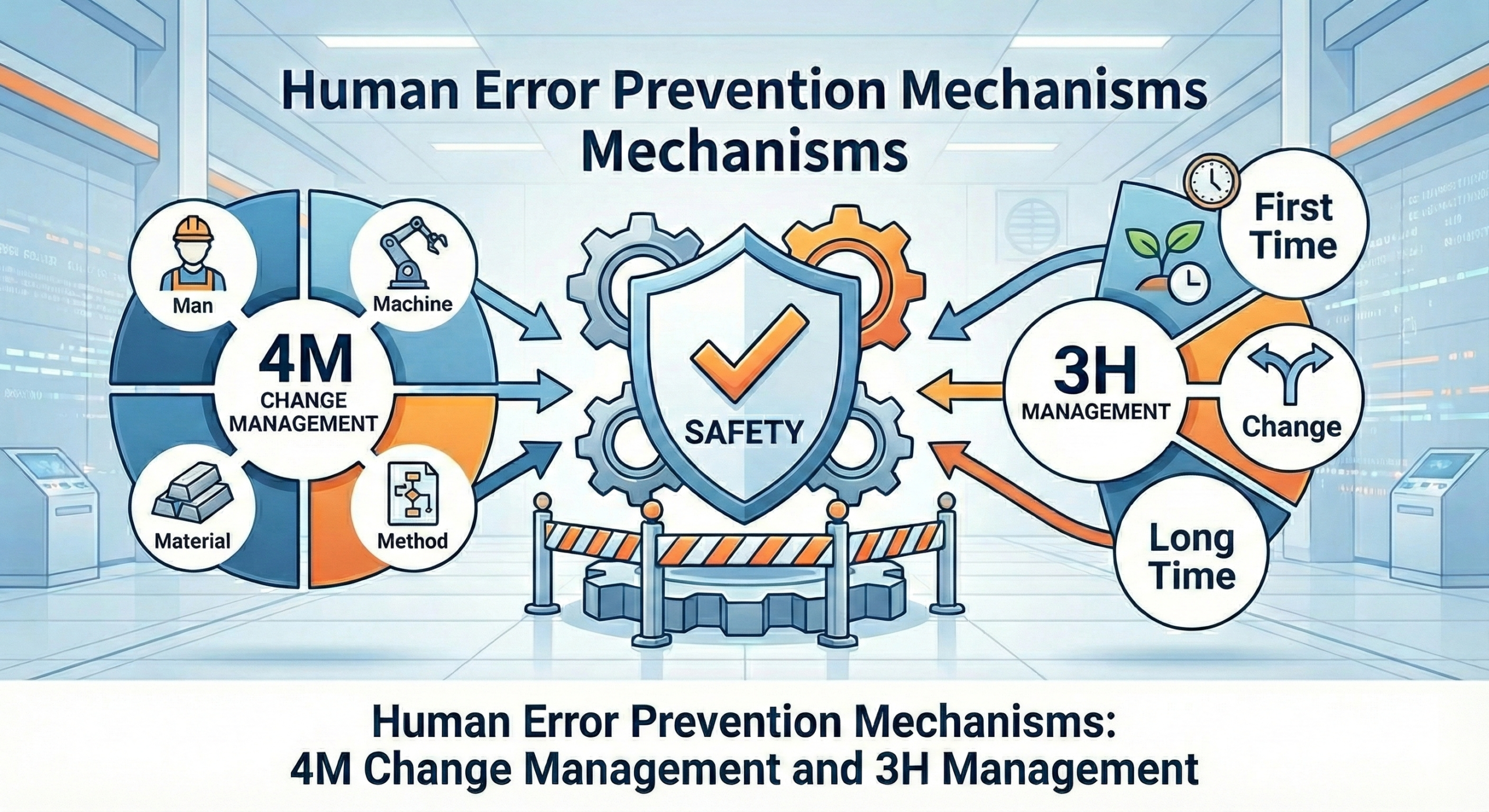
Mechanisms to Prevent Human Error: 4M Change Management and 3H Management
A Practical Approach in Pharmaceutical Manufacturing
At a morning meeting in a pharmaceutical plant, the manufacturing director began with a grave expression: “During last night’s shift, a weighing error occurred with the active pharmaceutical ingredient. Fortunately, we discovered it before shipment, but if it had reached the market…” Such scenarios represent a reality that can occur at any pharmaceutical manufacturing facility.
In pharmaceutical manufacturing, human error cannot be dismissed as merely a quality issue. It harbors the potential to become a critical incident directly connected to patient health and, in some cases, to life itself. If the amount of active ingredient contained in a single tablet deviates from specifications, not only may the therapeutic effect be lost, but there is also a risk of adverse effects from overdosing. Should microbial contamination occur during the manufacturing process of sterile preparations, there is a danger of causing serious infections.
Against this background, GMP (Good Manufacturing Practice) positions the prevention of human error as central to the quality assurance system. This article explains two methodologies practiced in pharmaceutical plants—”4M Change Management” and “3H Management”—incorporating actual field experience and case studies.
1. The Reality of Human Error in Pharmaceutical Plants
1.1 Why Do Errors Occur in Pharmaceutical Plants?
Let me introduce an actual case from a pharmaceutical plant. An experienced operator was weighing active pharmaceutical ingredients in the same manner as always. However, on that day, fatigue had accumulated from overtime continuing from the previous day, and due to a sudden change in the production schedule, the work was being carried out in a different sequence than usual. As a result, active pharmaceutical ingredients with similar names were confused, and the wrong raw material was used. This error was discovered through analysis by the quality control department, but manufacturing of one lot had already been completed, leading to a significant loss involving product disposal on the scale of tens of millions of yen (hundreds of thousands of dollars).
As this case demonstrates, human error in pharmaceutical plants is not caused by simple carelessness alone. It often occurs when multiple factors overlap, such as fatigue, sudden changes, and confusion due to similar names. When such accidents occur, it is not uncommon for losses on the scale of tens of millions of yen to occur due to disposal of one product lot. Furthermore, factors specific to pharmaceutical plants—such as the constrained working environment inside cleanrooms, strict time management, complex manufacturing processes, and the ever-present pressure of regulatory agency compliance—increase the risk of errors.
1.2 GMP’s Approach to Error Prevention
With the revision of the Pharmaceutical and Medical Device Act (PMD Act) in Japan through 2024 and ongoing updates into 2025, manufacturing and marketing authorization holders are now required to maintain even more stringent quality management systems than before. Particularly noteworthy is that the documentation and continuous improvement of human error prevention measures have been clearly mandated.
The fundamental philosophy of GMP is based on the premise that “humans will inevitably make mistakes.” Therefore, rather than depending on individual attentiveness, the construction of a system that prevents errors as a system is required. Specifically, the following are mandated: thorough education and training of workers with periodic evaluation of their competency; establishment of clear and easily understandable standard operating procedures (SOPs); when errors occur, investigation of the root cause and reliable implementation of corrective and preventive actions (CAPA); and evaluation of all changes in advance with appropriate approval processes.
Current international GMP guidelines, including ICH Q10 (Pharmaceutical Quality System), emphasize a risk-based approach to change management and continuous process verification. The PIC/S (Pharmaceutical Inspection Co-operation Scheme) guidelines, which have been widely adopted globally, further reinforce the systematic approach to error prevention through robust change control systems.
2. Practical Implementation of 4M Change Management in Pharmaceutical Plants
2.1 The Essential Nature of the 4M Concept
In quality control at pharmaceutical plants, the concept of 4M is used daily, and understanding its essence is crucial. 4M is an acronym for the four critical elements that affect manufacturing: Man (people), Machine (equipment and facilities), Material (materials), and Method (methods).
In pharmaceutical plants, “Man” refers not only to manufacturing operators but to all people involved in pharmaceutical manufacturing, including quality control personnel, validation specialists, and cleanroom workers. “Machine” encompasses diverse equipment such as tablet presses that form tablets, filling machines that fill injectable preparations, sterilizers that sterilize products, and HPLC (High-Performance Liquid Chromatography) systems that analyze quality. “Material” is a comprehensive concept that includes not only direct materials such as active pharmaceutical ingredients (APIs) and excipients but also packaging materials, cleaning agents, and reagents. “Method” means all documents and procedures that define working methods, such as manufacturing instructions, SOPs, validation protocols, and analytical methods.
These four elements do not exist independently but are closely interrelated. When a change occurs in one element, the impact ripples to other elements, and errors may occur in unexpected places.
The interaction between these elements can be illustrated as follows:
| Change Element | Primary Impact | Secondary Impact | Potential Error Risk |
| Man (Personnel change) | Skill variation | Process execution difference | Incorrect operation, deviation from SOP |
| Machine (Equipment modification) | Process parameter change | Product quality variation | Out-of-specification results, contamination |
| Material (Raw material change) | Physical/chemical property difference | Processing condition adjustment needed | Formulation failure, stability issues |
| Method (Procedure update) | Work flow change | Training requirement | Misunderstanding, incomplete execution |
2.2 The Reality of Change Management Systems
In GMP, change control is a mandatory requirement. All changes must be evaluated for their impact on quality and must receive appropriate approval. While this requirement may seem cumbersome, the importance becomes clear when examining actual cases that have occurred in pharmaceutical plants.
At one pharmaceutical plant, the punch and die of a tablet press on the tablet manufacturing line became worn and required replacement. What seemed like a simple parts replacement was subjected to careful impact assessment by the quality assurance department. Multifaceted examination was necessary, including the possibility that the new punch and die could change tablet hardness, effects on disintegration properties, consistency with already validated parameters, and impacts on stability studies.
The change request form first receives confirmation from the manufacturing department head, then from the QA department head, and ultimately approval from the quality assurance manager. This process takes time, but checks from different perspectives at each stage prevent oversights. After the actual punch and die replacement, the first lot is managed intensively, and normal production begins only after confirming that all quality items are within specifications.
In accordance with current FDA guidance on “Changes to an Approved NDA or ANDA” (revised 2023), pharmaceutical manufacturers must categorize changes based on their potential impact on product quality, safety, and efficacy. This risk-based approach helps prioritize resources and ensures appropriate regulatory notification or approval is obtained.
2.3 Learning from an Example of Active Pharmaceutical Ingredient Supplier Change
Let’s examine in detail an actual case of changing an active pharmaceutical ingredient supplier. For a major product of a certain pharmaceutical company, consideration began for switching from an overseas manufacturer to a domestic manufacturer from the perspectives of supply stability and cost reduction.
First, the quality control department began detailed analysis of the new active pharmaceutical ingredient. Comparison of impurity profiles involved precise analysis of the types and amounts of impurities contained to confirm equivalence with the existing product. Confirmation of particle size distribution and crystal form evaluated the impact of physical properties of the active pharmaceutical ingredient on the formulation process. Analysis of residual solvents confirmed that the types and amounts of solvents used were within specifications.
During this evaluation process, it was discovered that the new active pharmaceutical ingredient had somewhat larger particle size, with the possibility that penetration of the binder in the granulation process might be insufficient. Therefore, after consultation with the manufacturing department, optimization of granulation conditions was undertaken. Specifically, the binder amount was increased by 5% from the conventional formulation, and the supply air temperature of the fluid bed granulator was raised by 5°C, making appropriate granulation possible.
Accompanying this change, two hours of classroom education were provided to all operators, followed by practical training. The education explained in detail why the change was necessary, what points required attention, and how to respond if abnormalities occurred.
For validation, three lots were manufactured under the new conditions, confirming that all quality items were within specifications. Furthermore, accelerated stability studies (6 months at 40°C, 75% relative humidity) and long-term stability studies (36 months at 25°C, 60% relative humidity) were initiated to confirm stability of quality over time.
Through this series of efforts, while maintaining quality within specifications after the change, stabilization of active pharmaceutical ingredient procurement and significant cost reduction were achieved.
This approach aligns with ICH Q11 guidelines on “Development and Manufacture of Drug Substances,” which emphasizes the importance of understanding the relationship between drug substance attributes and drug product performance. The establishment of a control strategy that encompasses both the API supplier qualification and ongoing quality monitoring is essential for successful supplier changes.
2.4 Comprehensive Management in Sterile Filling Line Renewal
In the manufacture of injectable preparations, ensuring sterility is the most critical quality element. From a case of updating an aging sterile filling line with the latest equipment, let’s examine how a change in Machine (equipment) affects the other three M elements.
The new sterile filling machine improved filling accuracy from ±3% to ±1% compared to the conventional system, and filling speed doubled from 100 vials per minute to 200 vials per minute. Furthermore, by adopting an isolator system, it became possible to minimize contact opportunities between workers and products.
However, this equipment renewal was not merely a machine replacement. First, regarding human elements, glove operation inside the isolator required completely different techniques from conventional work in open systems. Therefore, a new operator certification system was introduced, implementing 40 hours of glove operation proficiency training. As confirmation of aseptic operations, media fill tests using culture medium instead of actual products were conducted to prove that each worker could work aseptically.
In terms of materials, confirmation of rubber stopper compatibility was necessary. Because the needle thickness and speed of the new filling machine changed, it was necessary to evaluate the impact on rubber stoppers and optimize the amount of silicone oil coating. The vial supply method was also modified to match the new equipment.
In terms of methods, new SOPs were created for 15 documents, the environmental monitoring plan was revised, and process control values were reset. These documents were refined into practical ones suited to actual field conditions through repeated revisions while performing actual work.
The implementation of isolator technology represents a significant advancement in aseptic processing, as outlined in the FDA’s “Guidance for Industry: Sterile Drug Products Produced by Aseptic Processing — Current Good Manufacturing Practice” (2004, with continued relevance). The use of restricted access barrier systems (RABS) or isolators has become the industry standard for minimizing human intervention and enhancing product sterility assurance.
2.5 Validation and Continuous Monitoring Requirements
Following major equipment changes such as the sterile filling line renewal, comprehensive validation activities must be conducted in accordance with current regulatory expectations. The validation approach should include:
Installation Qualification (IQ): Verification that the equipment is installed according to specifications and that all utilities, instruments, and ancillary systems meet design requirements.
Operational Qualification (OQ): Demonstration that the equipment operates according to its operational specifications across all anticipated operating ranges.
Performance Qualification (PQ): Evidence that the process consistently produces results meeting predetermined acceptance criteria when operating under normal conditions.
Modern regulatory guidance, particularly FDA’s Process Validation guidance (2011) and EU GMP Annex 15 on Qualification and Validation, emphasizes a lifecycle approach to validation. This includes three stages:
- Process Design: Understanding the process through development studies and risk assessment
- Process Qualification: Confirming that the process design is capable of commercial manufacturing
- Continued Process Verification: Ongoing assurance that the process remains in a state of control
For the sterile filling line example, continued process verification would include:
- Regular media fill studies to confirm continued sterility assurance
- Trending of critical process parameters and quality attributes
- Annual product quality reviews to identify any drift in performance
- Periodic requalification based on a risk-based schedule
3. The 3H Management Approach: Addressing Human Factors Systematically
3.1 Understanding the 3H Concept in Pharmaceutical Context
While the original document mentions 3H management in the title, it is important to elaborate on this critical concept. The 3H approach addresses three specific human-related factors that significantly contribute to errors in pharmaceutical manufacturing:
Hajimete (初めて – First Time): Situations where operators perform a task for the first time or after a long interval. This includes new employees, personnel assigned to different tasks, or execution of infrequent operations such as annual equipment maintenance or validation activities.
Henkō (変更 – Change): Any modification to established processes, procedures, equipment, materials, or personnel. This directly links to the 4M change management discussed earlier but specifically focuses on the human impact of changes.
Hisashiburi (久しぶり – After a Long Time): Operations performed infrequently, where skills may have deteriorated or procedural knowledge may have faded. Examples include seasonal production campaigns, annual cleaning validation, or rarely performed troubleshooting procedures.
3.2 Practical Implementation of 3H Management
The systematic management of 3H situations requires specific organizational approaches:
For Hajimete (First Time) situations:
Pharmaceutical companies implement structured training programs that include initial classroom instruction, supervised practical training, and formal competency assessment before operators can work independently. A pharmaceutical plant producing sterile products might require new operators to complete 160 hours of training, including 40 hours on aseptic techniques, before they are certified to work in Grade A/B environments.
Documentation plays a crucial role. Each operator maintains a training record that tracks all completed training modules, dates of competency assessments, and requalification schedules. When introducing a new analytical method, for example, quality control analysts would complete method-specific training and perform a minimum of three successful executions under supervision before independent operation.
For Henkō (Change) situations:
Change management systems must incorporate specific provisions for managing the human element of change. When a manufacturing procedure is revised, the change control process should include:
- Impact assessment on operator workload and complexity
- Identification of all affected personnel
- Design of appropriate training interventions
- Supervised execution during initial implementation
- Feedback collection from operators to refine procedures
A practical example: When a tablet coating process was modified to improve appearance, operators received training on the new spray rate settings, were provided with visual standards showing acceptable vs. unacceptable coating quality, and the first five production batches were conducted with additional supervision and quality checks.
For Hisashiburi (Long Time) situations:
Organizations address infrequent operations through several mechanisms:
Refresher training programs are scheduled based on the frequency of task performance. For operations performed quarterly or less frequently, operators complete abbreviated training sessions before each execution. This might include reviewing the relevant SOP, watching a demonstration video, and discussing potential problems with a supervisor.
Enhanced procedural support is provided for infrequent activities. Some pharmaceutical plants use detailed photographic work instructions or even video guidance for complex, infrequent operations. For example, annual filter integrity testing might be supported by a video showing each step of the process.
Buddy systems pair experienced personnel with those performing infrequent tasks to provide real-time guidance and serve as a second check against errors.
3.3 Integration of 4M and 3H Management Systems
The power of combining 4M change management with 3H risk factor management creates a comprehensive error prevention system. Consider how these approaches work together:
When a pharmaceutical company decided to implement a new automated inspection system for parenteral products (a Machine change in 4M terms), the project team recognized multiple 3H triggers:
- Hajimete: Operators would be using the new inspection technology for the first time
- Henkō: The inspection method itself was changing from manual to automated
- Hisashiburi: Some operators had not received training on automated systems since their initial employment years ago
The integrated management approach included:
- Formal change control documentation assessing impacts across all 4M elements
- Specialized 3H risk assessment identifying specific training and support needs
- Extended training program (80 hours vs. normal 40 hours) recognizing the Hajimete condition
- Parallel running of old and new systems during transition to address Henkō risks
- Refresher training on automation principles for personnel in the Hisashiburi category
- Enhanced supervision and checking during the first three months of operation
This comprehensive approach resulted in successful implementation with zero product quality incidents during the transition period.
3.4 Measuring the Effectiveness of Error Prevention Systems
Pharmaceutical companies must establish metrics to evaluate the effectiveness of their 4M and 3H management systems. Key performance indicators might include:
Leading Indicators (predictive measures):
- Percentage of changes completed with full 4M impact assessment
- Training completion rates for personnel in 3H situations
- Number of near-misses identified and addressed
- Frequency of procedure reviews and updates
- Participation rates in continuous improvement activities
Lagging Indicators (outcome measures):
- Number of deviations per 1,000 operations
- Number of out-of-specification results
- Product complaints per million units produced
- Batch rejection rate
- Regulatory observations related to human error
A well-managed pharmaceutical facility might track these metrics monthly, with trending analysis to identify areas requiring enhanced focus. For example, if deviations increase following a specific type of change, the organization might strengthen the corresponding change management procedures.
3.5 The Role of Technology in Supporting Error Prevention
Modern pharmaceutical manufacturing increasingly leverages technology to support both 4M change management and 3H risk mitigation:
Electronic Quality Management Systems (eQMS): These systems automate change control workflows, ensure all required approvals are obtained, maintain complete audit trails, and link related documents and training records. When a change is initiated, the system can automatically identify all affected documents, generate training requirements, and track completion.
Manufacturing Execution Systems (MES): These systems provide electronic batch records that guide operators through procedures step-by-step, prevent out-of-sequence operations, and require checkpoints at critical steps. For operators in Hajimete or Hisashiburi situations, the system provides additional guidance and may require supervisory approval before proceeding.
Learning Management Systems (LMS): These track all training activities, automatically notify personnel of upcoming requalification requirements, and can deliver computer-based training modules. When a change occurs affecting multiple documents, the LMS automatically assigns appropriate training to all affected personnel.
Artificial Intelligence and Machine Learning: Emerging applications include predictive analytics to identify conditions likely to lead to errors, pattern recognition in deviation data to identify systemic issues, and natural language processing to analyze investigation reports and identify common root causes.
However, technology is an enabler, not a substitute for robust systems and engaged personnel. The most successful pharmaceutical operations combine strong procedural frameworks with appropriate technological support and a culture that values quality and continuous improvement.
4. Building a Culture of Error Prevention
4.1 The Human Factor Beyond Systems and Procedures
While 4M change management and 3H management provide systematic frameworks for error prevention, their effectiveness ultimately depends on organizational culture. A pharmaceutical plant may have perfectly documented procedures, but if personnel do not understand the rationale behind them or feel pressured to prioritize speed over quality, errors will occur.
Leading pharmaceutical companies recognize that building a quality culture requires:
Psychological Safety: Workers must feel comfortable reporting errors, near-misses, and concerns without fear of punishment. When an operator at a European pharmaceutical facility nearly used the wrong raw material but caught the error before addition, she immediately reported it. Rather than facing discipline, the company recognized her alertness, investigated the system failures that allowed the near-miss, and implemented improvements. This response reinforced to all employees that reporting problems is valued.
Visible Leadership Commitment: When quality leaders regularly visit manufacturing areas, participate in deviation investigations, and recognize personnel who identify problems, they send a clear message about priorities. One pharmaceutical CEO makes it a practice to personally call employees who report significant near-misses to thank them for their vigilance.
Continuous Learning Mindset: Organizations that treat errors as opportunities for system improvement rather than individual failures develop more robust processes. This includes conducting thorough root cause investigations, sharing learnings across sites and departments, and implementing preventive actions broadly rather than addressing only the immediate problem.
4.2 Regulatory Expectations and Industry Trends
The regulatory landscape continues to evolve toward more sophisticated approaches to quality management and error prevention:
FDA’s Quality Metrics Initiative: This voluntary program encourages pharmaceutical manufacturers to submit quality metrics data, promoting industry-wide learning and enabling comparative assessment of quality system effectiveness.
ICH Q12 (Technical and Regulatory Considerations for Pharmaceutical Product Lifecycle Management): This guideline, implemented since 2019, facilitates the management of post-approval chemistry, manufacturing, and controls (CMC) changes through established conditions and enables more efficient change management.
Enhanced Process Understanding: Regulatory agencies increasingly expect manufacturers to demonstrate deep understanding of their processes through Quality by Design (QbD) principles, with well-defined critical quality attributes (CQAs), critical process parameters (CPPs), and design spaces.
Digital Transformation: Regulatory authorities are developing frameworks for pharmaceutical 4.0 technologies, including continuous manufacturing, real-time release testing, and data integrity considerations for increasingly electronic quality systems.
Industry associations such as ISPE (International Society for Pharmaceutical Engineering) and PDA (Parenteral Drug Association) provide forums for sharing best practices and developing industry guidance on emerging topics related to error prevention and quality systems.
5. Practical Recommendations for Implementation
For pharmaceutical organizations seeking to strengthen their error prevention systems through 4M change management and 3H management, consider the following roadmap:
Assessment Phase (1-2 months):
- Review existing change control procedures against current regulatory guidance
- Analyze deviation and investigation data to identify patterns and common root causes
- Survey personnel to understand their perceptions of system effectiveness and barriers to compliance
- Benchmark against industry best practices
Design Phase (2-3 months):
- Develop or revise change control procedures incorporating comprehensive 4M assessment
- Create 3H identification and management protocols
- Design training programs for personnel at all levels
- Establish metrics and monitoring systems
- Select and configure supporting technology platforms
Implementation Phase (6-12 months):
- Pilot the enhanced system in a limited area to refine procedures
- Train all relevant personnel on new or revised procedures
- Implement supporting technology
- Establish regular review and continuous improvement processes
- Communicate progress and celebrate successes
Sustainment Phase (ongoing):
- Monitor metrics and trends to identify opportunities for improvement
- Conduct periodic system audits to ensure ongoing compliance
- Update procedures based on regulatory changes and lessons learned
- Maintain personnel competency through ongoing training
- Share learnings across the organization
Success requires executive sponsorship, cross-functional collaboration, and sustained commitment. Organizations that view quality systems as a competitive advantage rather than a compliance burden typically achieve superior results.
Conclusion
In pharmaceutical manufacturing, where products directly impact patient health and safety, preventing human error is not optional—it is a fundamental responsibility. The systematic approaches of 4M change management and 3H management, when properly implemented and supported by strong organizational culture and appropriate technology, provide powerful frameworks for minimizing error risk.
These methodologies recognize the complexity of pharmaceutical operations and the reality that errors typically result from system failures rather than individual incompetence. By systematically evaluating changes across all relevant dimensions (Man, Machine, Material, Method) and providing targeted support for high-risk human situations (First time, Change, After a long time), pharmaceutical organizations can significantly reduce error rates while improving operational efficiency.
As regulatory expectations continue to evolve and manufacturing technologies advance, the principles underlying these error prevention systems remain constant: understand your processes thoroughly, assess changes systematically, support personnel effectively, learn from problems, and continuously improve. Organizations that embrace these principles and implement them with discipline and commitment will excel in fulfilling their mission of reliably delivering high-quality medicines to patients who depend on them.
The case studies and examples presented in this article demonstrate that while implementing robust error prevention systems requires significant effort and resources, the benefits—in terms of patient safety, product quality, regulatory compliance, and operational efficiency—far outweigh the costs. As one quality director stated, “We cannot afford not to invest in preventing errors. The real cost is not in building these systems, but in the consequences of failing to do so.”
Note: This article reflects practices and regulatory requirements as of early 2025. Readers should verify current regulatory expectations and guidance for their specific jurisdictions and applications.

Comment