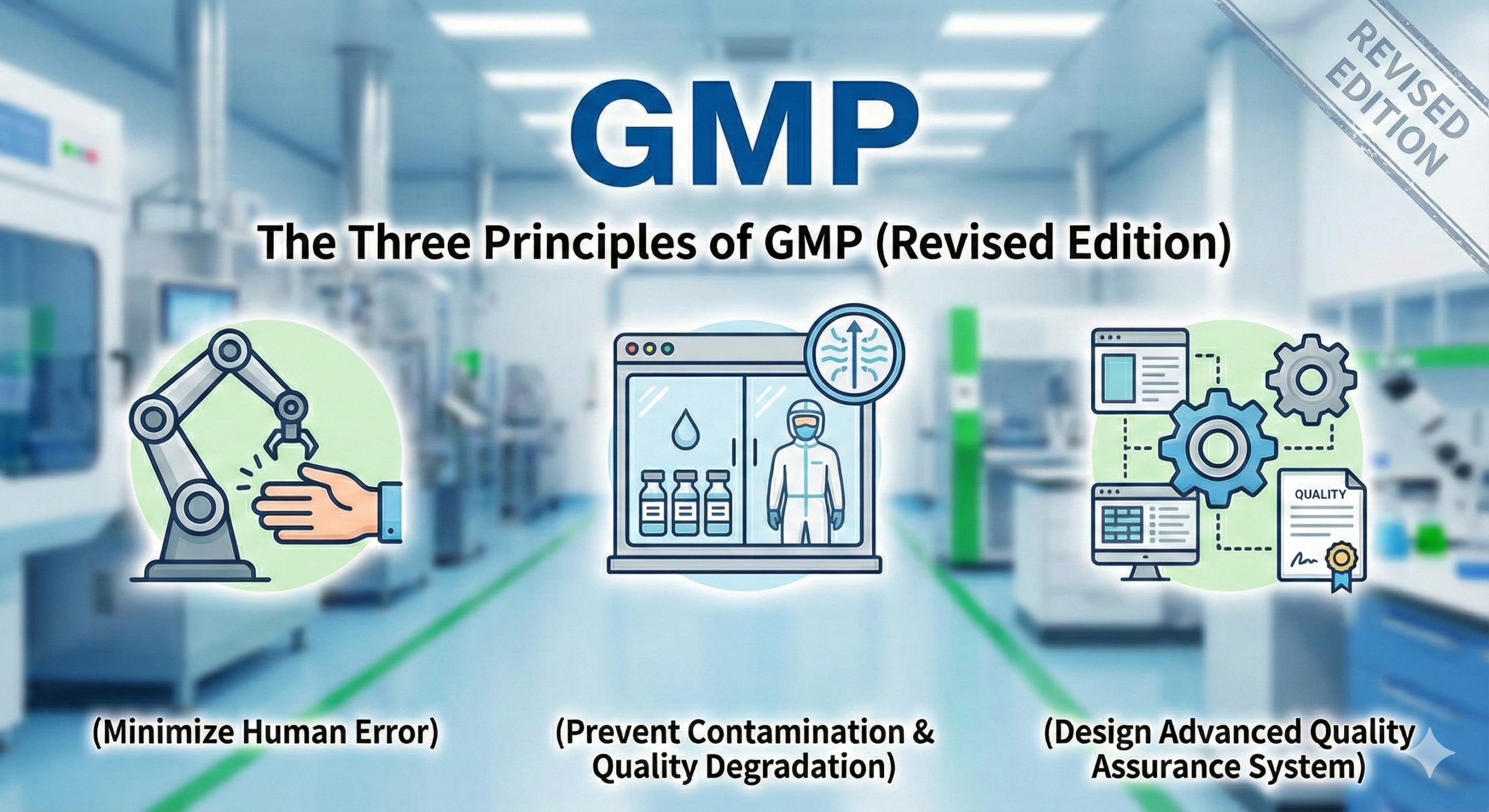
The Three Principles of GMP (Revised Edition)
What Are the Three Principles of GMP?
The three principles of GMP are as follows:
- Minimize human error
- Prevent contamination and quality deterioration
- Design systems to ensure higher quality assurance
These principles are widely recognized in pharmaceutical manufacturing. It is believed that they were used to explain the fundamental philosophy of pharmaceutical GMP in an easily understandable manner when it was introduced in Japan. Interestingly, the expression “three principles” is not explicitly stated in regulatory requirements or official notifications, and no clear record remains as to who first proposed them. Nevertheless, these principles accurately express the essence of pharmaceutical manufacturing and continue to function as important guidelines in the industry today.
International Perspectives
While the fundamental concepts of GMP are internationally consistent, their expression may vary among countries and international organizations.
The U.S. FDA Approach
In the United States, cGMP (current Good Manufacturing Practice), defined in federal regulations 21 CFR Parts 210 and 211, serves as the standard for pharmaceutical manufacturing. The FDA emphasizes continuous improvement, risk management, process control, and data integrity, requiring manufacturers to adopt the latest scientific knowledge and technology. In American GMP culture, the concepts of “documentation,” “verification,” and “maintaining cleanliness” are strongly emphasized, which are essentially common with Japan’s three principles.
Development of WHO GMP
In 1969, the World Health Organization (WHO) recommended that member countries adopt and implement a GMP-based certification system in pharmaceutical trade. WHO’s GMP guidelines are currently used by pharmaceutical regulatory authorities and the pharmaceutical industry in over 100 countries, playing a particularly important role as standards for ensuring pharmaceutical quality in developing nations. WHO GMP integrates philosophical elements of quality assurance with practical requirements for manufacturing and quality control, encompassing major components such as personnel, premises, equipment, materials, documentation, and validation.
Details of Japan’s Three Principles of GMP
The intentions behind Japan’s three principles of GMP are as follows:
1. Minimize Human Error
This principle addresses “human error,” one of the greatest risk factors in manufacturing.
Main Implementation Methods:
- Creation and strict adherence to Standard Operating Procedures (SOPs)
- Implementation of systematic training programs
- Establishment of double-check systems for critical processes
- Personnel qualification assessment and continuous competency maintenance
- Standardization of operations to ensure consistent product quality regardless of who performs the work
2. Prevent Contamination and Quality Deterioration
To maintain pharmaceutical quality, it is necessary to thoroughly manage contamination risks in the manufacturing environment and processes.
Main Implementation Methods:
- Cross-contamination prevention measures (dedicated facilities, campaign production, appropriate zoning, etc.)
- Cleaning and cleaning validation
- Reliable implementation of line clearance
- Regular maintenance and calibration of equipment and facilities
- Environmental monitoring (temperature, humidity, cleanliness, microbial control, etc.)
- Appropriate storage management of raw materials and intermediate products
3. Design Systems to Ensure Higher Quality Assurance
This principle requires not merely following rules but establishing a quality assurance system based on continuous improvement and scientific evidence.
Main Implementation Methods:
- Establishment of deviation management systems and root cause analysis
- Appropriate implementation of change control
- Regular conduct of Product Quality Reviews
- Continuous improvement of quality systems through management reviews
- Introduction of Pharmaceutical Quality Systems (PQS)
- Utilization of Quality Risk Management
- Ensuring data integrity
Historical Background of GMP
The Thalidomide Tragedy and Regulatory Turning Point
The origins of GMP lie in the tragic history of serious health damage caused by pharmaceuticals. In particular, the thalidomide tragedy that occurred between 1957 and 1962 had a decisive impact on pharmaceutical regulations worldwide.
Thalidomide was launched as a sleeping pill in West Germany in 1957 and was used as a “safe drug” for treating morning sickness in pregnant women. However, it was discovered that when taken by pregnant women in early pregnancy, it caused severe limb malformations and hearing impairments in fetuses. Following the Lenz warning in November 1961, sales suspension and recall measures were implemented in countries worldwide. However, in Japan, there was approximately a 10-month delay until sales were suspended in September 1962, resulting in expanded damage.
Legislation of GMP in the United States
Following the thalidomide tragedy, the Kefauver-Harris Amendment was enacted in the United States in 1962, making proof of efficacy mandatory for drug approval. Furthermore, in 1963, the FDA became the world’s first to legislate GMP, establishing standards for facilities, manufacturing control, and quality control in pharmaceutical manufacturing. This was based on the recognition that managing the manufacturing process itself, not just final product testing and inspection, is essential for ensuring pharmaceutical quality.
International Development of GMP
In 1969, WHO established GMP and, at the 22nd World Health Assembly, recommended that member countries adopt and implement a GMP-based certification system in pharmaceutical trade. This recommendation led to GMP spreading to countries worldwide as an international standard for pharmaceutical quality assurance.
Introduction and Development of GMP in Japan
In Japan, preparations for establishing and implementing GMP began around 1972, centered on the Pharmaceutical Affairs Bureau of the Ministry of Health and Welfare. On September 14, 1974, the “Standards Concerning Manufacturing and Quality Control of Pharmaceuticals” (notification from the Director of the Pharmaceutical Affairs Bureau of the Ministry of Health and Welfare) was issued to prefectures and implemented as administrative guidance from April 1976. It is believed that WHO’s GMP requirements were referenced at this time.
Subsequently, in 1980, it was legislated as the “Ministerial Ordinance on Standards for Manufacturing Control and Quality Control of Drugs and Quasi-drugs” (GMP Ministerial Ordinance). In 1994, it became a requirement for manufacturing licenses, and in 2005, it became a requirement for marketing authorization approval, with its scope and importance gradually expanding.
Recent Regulatory Trends
2021 Revised GMP Ministerial Ordinance
On August 1, 2021, significantly revised GMP Ministerial Ordinance was enforced for the first time in approximately 17 years. This revision primarily aims to ensure international harmonization and address recent quality issues.
Main Revision Points:
- Introduction of Pharmaceutical Quality System (PQS): Mandated establishment of comprehensive quality assurance systems at manufacturing sites
- Codification of Data Integrity Requirements: Ensuring authenticity, accuracy, completeness, and availability of records
- Legislation of Quality Risk Management: Introduction of risk-based approaches based on ICH Q9
- Strengthening of Product Quality Review: Promotion of regular quality reviews and continuous improvement
- Compliance with Approved Matters: Clarification of manufacturers’ responsible involvement in approved matters
- Supplier Management for Materials: Quality assurance across the entire supply chain
Joining PIC/S and International Harmonization
Japan joined PIC/S (Pharmaceutical Inspection Co-operation Scheme) in July 2014. PIC/S is a cooperative framework aimed at the international development, implementation, and maintenance of harmonized GMP standards and quality systems of inspection authorities, with over 50 countries currently participating.
By joining PIC/S, Japan’s GMP Ministerial Ordinance has been aligned with PIC/S GMP guidelines, advancing international mutual recognition. This has improved the reliability of quality assurance in the global distribution of pharmaceuticals.
Importance of Quality Culture in GMP
In recent years, regulatory authorities and the industry have emphasized the importance of “quality culture.” No matter how excellent systems and rules are established, true quality assurance cannot be achieved without the awareness and behavior of the people who operate them.
Quality culture is “the collection of beliefs, values, and behavioral norms shared by employees involved in quality” and includes the following elements:
- Attitude prioritizing patient safety
- High ethical standards and sense of justice
- Culture of openly discussing problems without concealment
- Commitment to continuous improvement
- Evidence-based decision-making
U.S. FDA officials have pointed out that “data integrity issues are more about quality culture than technical issues,” emphasizing the importance of top management positioning quality as a core value and sharing it throughout the organization.
Future Prospects
GMP needs to continuously evolve in response to scientific and technological progress, innovation in manufacturing technology, and advancing globalization. Topics attracting recent attention include:
Utilization of Advanced Technologies
- Process Analytical Technology (PAT): Process control through real-time monitoring
- Continuous Manufacturing: Transition from batch production to continuous production
- Application of Artificial Intelligence (AI) and Machine Learning: Utilization in data analysis, anomaly detection, predictive maintenance, etc.
- Digitalization: Promotion of electronic record and electronic signature systems and paperless operations
Implementation of Quality by Design (QbD)
The concept of “Quality by Design,” which builds quality from the design stage based on understanding of products and processes, is becoming widespread. This is systematized in ICH Q8 (Pharmaceutical Development), Q9 (Quality Risk Management), and Q10 (Pharmaceutical Quality System) guidelines, enabling more scientific and efficient quality assurance.
Addressing Supply Chain Complexity
With the globalization of manufacturing sites, supply chains from raw material procurement to product supply have become complex. In this environment, broader quality assurance than before is required, including supplier management, logistics management, and countermeasures against counterfeit pharmaceuticals.
Conclusion
The three principles of GMP concisely express the essence of quality assurance in pharmaceutical manufacturing, and their importance remains unchanged today. However, GMP is never static but continuously develops in response to scientific and technological progress, societal demands, and changes in the regulatory environment.
All people engaged in the pharmaceutical industry are required to understand the historical background and fundamental philosophy of GMP, comply with the latest regulatory requirements, strive to foster quality culture, and maintain an attitude that prioritizes patient safety above all. This is our responsibility to never repeat tragedies like the thalidomide incident.

Comment