What is Digital Therapeutics (DTx)?
Digital Therapeutics (DTx, or digital therapy), which utilizes apps and other software to treat, for example, smartphone apps and IoT devices for therapeutic interventions for hypertension, diabetes, and neuropsychiatric disorders.
In 2010, WellDoc, a U.S. company, attracted attention when it received U.S. FDA (Food and Drug Administration/U.S. Food and Drug Administration) certification for its “Bluestar” treatment aid application for type 2 diabetes patients.
DTx is a software-based therapy that improves treatment outcomes through stand-alone or add-on use, and has already been put to some practical use in the United States, where it has been used for some time.
DTx is a new medical device product that was created about 10 years ago.
DTx will provide more treatment options for patients and physicians. Currently, the 3-hour wait for 5-minute treatment is chronic. However, with DTx, patients can receive treatment, care, and guidance at home without having to go to a medical facility. Patients can input symptoms and measurement data in real time, and doctors can use their “spare time” to examine and instruct patients.
In the industrial world, the number of start-up ventures developing DTx is increasing. The author has received endless inquiries from many venture companies and software developers who want to enter the medical device industry.
On the other hand, for pharmaceutical companies, this could be a source of non-pharmaceutical revenue. In the past, pharmaceutical companies had to invest huge amounts of money for 10 to 15 years to develop new drugs. In addition, it is not uncommon for a drug to be discontinued in the middle of development. In other words, it is like a “one or two chance” game. Moreover, even if a drug was lucky enough to be launched on the market, generic versions would appear on the market due to patent term issues, and so the development of new drugs had to be constantly repeated.
Unlike pharmaceuticals, DTx can be developed in a relatively short period of time. Moreover, it is relatively easy to add or change functions after the product is launched.
Pioneer of DTx: “Prescribed Apps”Bluestar (WellDoc)
DTx came to prominence in 2010 when the FDA approved medical device software called Bluestar, developed by WellDoc, as a “prescribed app” to assist in the self-management of type 2 diabetes.
A “prescribed app” is one that can be used by a physician who issues a code called a “release key” to the patient, who then enters the code into the app. In other words, it is an alternative to a prescription.
Bluestar was approved by the FDA in 2010 after large-scale clinical trials showed that it was as effective or more effective than new diabetes drugs and other pharmaceuticals.
Bluestar is actually a latecomer: the first DTx for type 2 diabetes was available, but it ran on a PC. This means that patients can now carry the medical device software with them at all times.
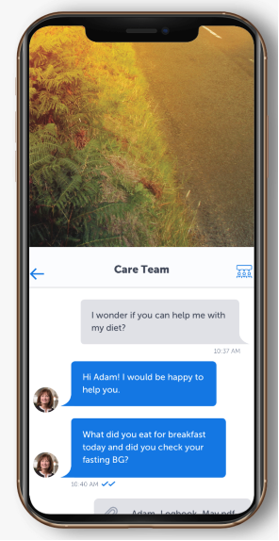
BlueStar’s function is to allow patients to record their blood glucose levels at home and display disease guidance and advice on lifestyle and motivation maintenance at appropriate times based on the input information. The app also allows users to ask questions to experts.
Furthermore, the system can learn about blood glucose control methods such as drug therapy, diet, and exercise therapy. On the other hand, for physicians, it can be a diagnostic support system, recording blood glucose levels, medications, and physical condition before each visit, and providing progress reports to the medical team.
“World’s first DTx prescribed for treatment” reSET(Pear Therapeutics Inc.
Developed by Pear Therapeutics, reSET demonstrates therapeutic efficacy against drug abuse and dependence through app-based cognitive behavioral therapy.
The difference is that BlueStar, described above, was approved as an aid to self-administration, whereas reSET was approved as a therapeutic measure.
The approved indications for reSET are patients 18 years of age or older receiving outpatient treatment for dependence on marijuana, cocaine, or alcohol.
A 12-week (90-day) treatment period is set, and a total of 61 different contents (therapy lessons) are provided, but it is recommended to proceed at a pace of about four per week with those related to your symptoms or recommended by your doctor.
A multicenter, open-label, randomized, controlled trial compared a group that received standard face-to-face counseling (control group) with a group that received less face-to-face counseling and used reSET in a population excluding opioid-dependent patients (399 patients). The reSET group was twice as likely to have a higher success rate of drug discontinuation than the control group. No adverse effects were reported during the trial.

Digital Therapeutics in Japan
In Japan, when the Pharmaceutical Affairs Law was revised in November 2014 and replaced by the Law Concerning Quality, Efficacy, and Safety Assurance of Drugs and Medical Devices (Pharmaceutical Affairs Law), “stand-alone programs (software)” were added to the list of covered medical devices. This opened the way for therapeutic applications to be prescribed by doctors and covered by health insurance.
In October 2017, the medical venture Cure Up announced the start of a clinical trial for a nicotine dependence treatment app (smoking cessation treatment app).
On May 30, 2019, the company announced that it had submitted an application for regulatory approval for a smartphone app to treat nicotine dependence. The application for the therapeutic app was the first in Japan and the first in the world for smoking cessation treatment; insurance coverage was approved on November 11, 2020.
A clinical trial (clinical trial) was conducted with 31 medical institutions in Japan, and the results were also presented. The study was conducted on 584 nicotine-dependent patients. Patients who used the app together increased their quit rate by 13 percentage points to 64%. The app was developed by Cure-Up in collaboration with Keio University School of Medicine.

For patients, quitting smoking and improving diabetes is a struggle against themselves. It can be difficult to quit smoking alone. Also, diabetes has no subjective symptoms, and people are often too busy to take their medications and treatments.
Thus, when the “heart breaks” during treatment, DTx support increases the likelihood of continuity. Thus, DTx seems like a dream come true. However, we have heard of many problems in conducting clinical trials to prove its effectiveness and in getting it covered by insurance. We will discuss these issues in another article.
related product
[blogcard url=https://xn--2lwu4a.jp/qms-md/ title=”QMS(手順書)ひな形 医療機器関連” ] [blogcard url= https://ecompliance.co.jp/SHOP/EL-010.html title=”【セミナービデオ】【手順書付き】医療機器ソフトウェア規制対応セミナー”] [blogcard url= https://ecompliance.co.jp/SHOP/O016.html title=”【VOD】DTx(デジタル医療)の最新の技術動向と知財戦略の新たな視点セミナー”] [blogcard url= https://ecompliance.co.jp/SHOP/L_MDCSV.html title=”【VOD】医療機器企業におけるCSV実践セミナー”] [blogcard url= https://ecompliance.co.jp/SHOP/MD-QMS-365.html title=”【IEC-62304対応】製品ソフトウェア設計開発手順書”]]]>


Comment